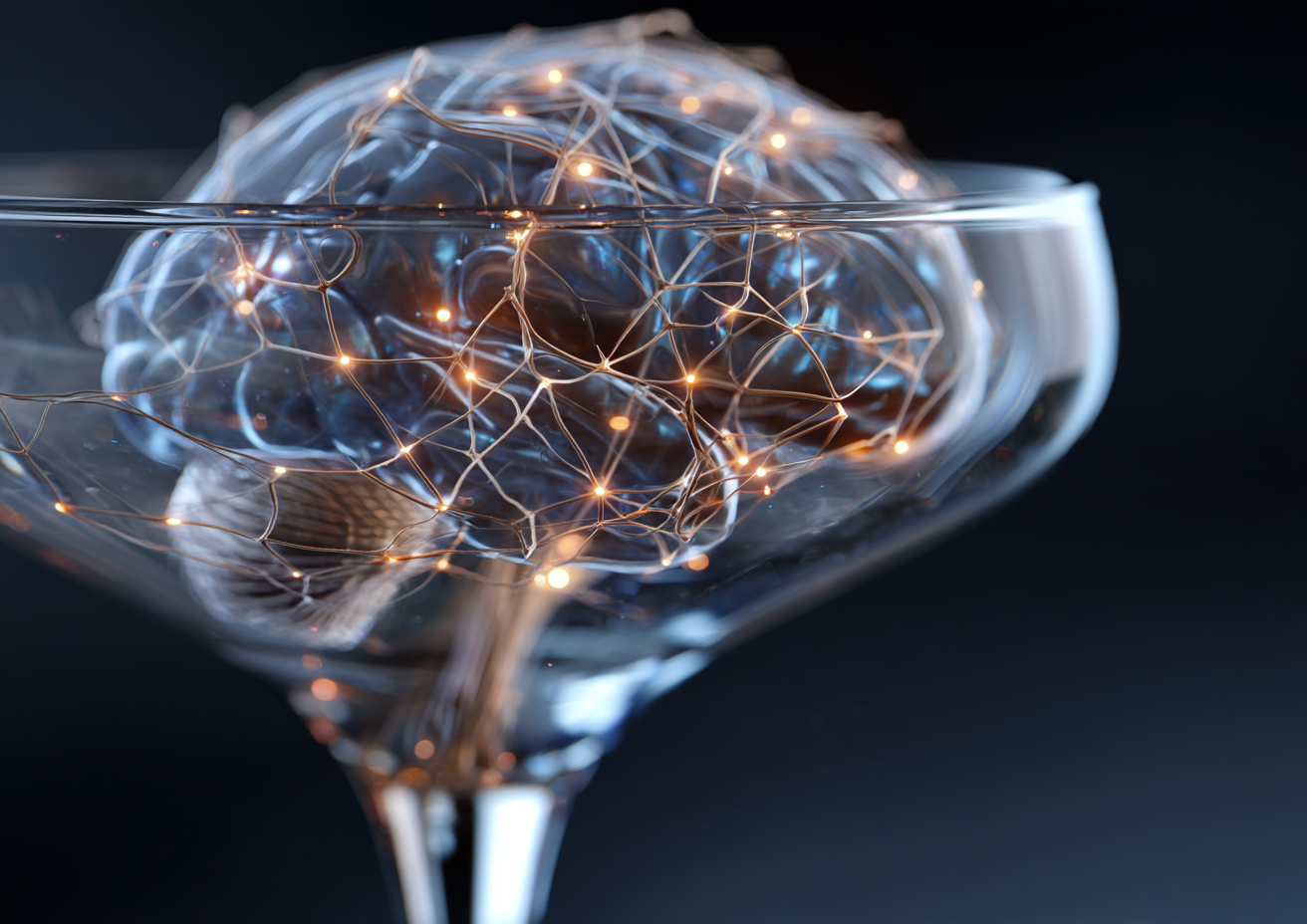
A recent study published in the Journal of Affective Disorders sheds light on the intersection of genetic risks and brain structure and function changes in major depressive disorder (MDD). For mental health providers, this research holds critical implications for understanding the biological mechanisms behind depression and enhancing patient outcomes.
Understanding Genetic Risks in Depression
Research indicates that genetics play a significant role in the vulnerability to depression. Genetic predisposition to depression often manifests as changes in the structure and functioning of key brain regions, such as the hippocampus, amygdala, and thalamus. These insights are essential for psychiatric professionals, including psychiatrists and psychiatric mental health nurse practitioners (PMHNPs), who seek to decipher the roots of MDD within their clinical practices.
Understanding these genetic factors equips clinical teams with the knowledge to tailor interventions. For instance, a family history of depression can guide decisions regarding more intensive therapeutic strategies during initial assessments.
Implications for Clinical Care Delivery
In clinical settings, recognizing how genetic factors affect brain structure can enhance operational efficiency. This knowledge can inform treatment plans in outpatient clinics and telepsychiatry models. For example, clinicians can utilize these insights to conduct targeted assessments for risk factors associated with MDD.
- Identify patients with a strong genetic history for proactive monitoring.
- Implement personalized treatment plans based on insights into brain structure alterations.
- Utilize genetic information to guide medication choices and therapeutic interventions.
Trends in Neurobiological Research
The ongoing studies around the genetic aspects of depression highlight the need for continuous education in the mental health field. Recognizing how genetic vulnerabilities manifest as structural changes in the brain allows mental health professionals to remain forward-thinking. Clinical psychologists, licensed clinical social workers (LCSWs), and board-certified behavior analysts (BCBAs) can leverage this information to formulate evidence-based practices that better address complex patient needs.
Additionally, as rehabilitation facilities and specialty care centers adopt more comprehensive approaches to MDD, integrating genetic insights will be crucial. This fosters an environment where professionals in various roles can collaborate effectively.
Addressing Operational and Regulatory Considerations
The study of depression genetics also implicates regulatory considerations within mental health practices. Ensuring compliance with evolving health regulations designed to address biological components of mental health care will be vital. Facilities must consider how findings influence policy development and patient care protocols.
Moreover, the operational realities of staffing mental health facilities can pose challenges. With a growing demand for skilled practitioners, organizations will need to innovate in attracting and retaining qualified professionals, such as psychiatrists and PMHNPs, who are knowledgeable about these new insights.
Fostering a Skilled Workforce
As mental health organizations adapt to these research findings, fostering a competent workforce becomes crucial. Employers should focus on creating training programs that educate staff about genetic predispositions to depression and their implications for clinical care.
- Develop continuous education programs focusing on genetic factors influencing mental health.
- Encourage interdisciplinary collaboration among clinical staff.
- Utilize telehealth for training sessions to maximize accessibility.
Staying abreast of current research allows mental health facilities to not only enhance patient care but also improve operational efficiencies. By understanding the connection between genetics and brain structure, clinical teams can better serve their populations while addressing the ongoing workforce challenges in the mental health sector.
Conclusion
In conclusion, the intersection of genetic predispositions and brain changes in major depressive disorder offers profound insights for mental health providers. Pulivarthi Group is dedicated to supporting organizations by providing access to hard-to-find mental health professionals across outpatient, inpatient, and specialty care settings. Our focus includes essential roles such as clinical psychologists, PMHNPs, BCBAs, psychiatric PA-Cs, LCSWs, and psychiatrists. By partnering with us, mental health facilities can enhance their service delivery and operational performance while navigating the complexities of patient care in light of new genetic research findings.